I find it refreshing that an article that speaks the truth and confronts the lies we have been brought up on about food. Dr. Michael Mosley says the following:
Once upon a time it all seemed incredibly clear. When I went to medical school in the early 1980s I was shown clogged up arteries, fresh from an autopsy, and was assured that this was the result of eating too much fat, particularly saturated fat, the sort found in red meat, milk, cheese and butter. Eating fat, we were told, raises your cholesterol levels and high levels of cholesterol are strongly linked to heart disease.
So I gave up butter and cheese and took to skimmed milk and zero-fat yoghurt. I told friends and family that eating fat would clog their arteries as surely as pouring lard down a drain. I also told my overweight father that the best way he could protect his waist, as well as his heart, was to go on a low-fat diet.
This was soon after he had been diagnosed as type 2 diabetic and started on medication. Following my advice he put aside the fats, ate more starchy foods – and got fatter and fatter. His diabetes also got steadily worse and he needed ever larger doses of medication to try and keep it under control. Twenty years later he died of heart failure, a common problem in diabetics, at the age of 74.
If I had known what I know now about the high failure rate of low-fat diets, my advice would have been completely different and he might have lived to see his grandchildren grow up.
Recently Britain’s National Obesity Forum and the Public Health Collaboration issued a report demanding a “major overhaul” of dietary guidelines – in particular claiming that the focus on low-fat diets, which has dominated dietary thinking for the last 40 years, has been a mistake.
It would be easy to dismiss this as another week, another confusing dietary claim. But from personal experience, and having spent many years looking into the science, I’m firmly on the side of the authors of this report.
So what led us to listen to the ”wrong” dietary advice for decades? The roots of current standard nutritional advice lie back in the 1950s, when an American scientist called Ancel Keys published a study into the association between diet and cardiovascular disease. His paper included a simple graph comparing fat consumption and deaths from heart disease in men from six different countries. Americans, who ate a lot of fat, were far more likely to get heart disease than the Japanese, who ate little fat. Case solved.
It is a myth that has taken a long time to die. Until very recently the American Heart Association was still issuing dire warnings about the dangers of eating foods containing cholesterol. Yet a meta-analysis of 17 studies published in the British Medical Journal in 2013 concluded that “higher consumption of eggs is not associated with increased risk of coronary heart disease or stroke”.
2013 also saw the publication of a hugely important study in the New England Journal of Medicine, which finally put a huge nail in the low-fat coffin.
For this trial, which started in 2003, Spanish researchers recruited over 7400 people, many of them Type 2 diabetics, and randomly allocated them to either a low-fat diet or a much higher fat “Mediterranean diet”, which along with fruit, vegetables and oily fish, encouraged them to eat oily nuts, olive oil and have a glass of wine with their meal.
The trial, due to run for many years, was stopped early because those on the higher fat, lower carb Mediterranean diet were doing so much better than those on the low-fat diet.
This became particularly relevant to me four years ago when I discovered that, like my father, I had become a type 2 diabetic while still in my early fifties. Rather than start on medication I invented a diet (the 5:2 diet), lost weight (10 kgs) and reversed my diabetes. Both my weight and my blood sugars have remained normal ever since. To keep them there I have taken up mindfulness (it reduces stress), I’ve become more active and, most of all, I have completely changed what I eat.
I cook with olive oil, eat full-fat yoghurt, snack on cheese and have switched back to butter. Eggs are a big part of my diet.
The reason, I believe, why this is a healthier diet than a low-fat one is because it keeps my insulin levels down. Because insulin is also a fat promoting hormone, advising people to eat lots of starchy foods (which is still standard dietary advice) is likely to make them fatter, not slimmer.
I’m not suggesting we should all start to glug down cream or gorge on stilton. What I do think is that official bodies need to urgently rethink their standard advice.
End of quote.
Being the suspicious and “sceptical bastard” I am, I see this diet as no accident, and if you look at the contents of processed foods, you see the evidence – lots of sugar and flour. It ain’t fats that make us fat. It’s SUGAR and refined carbs in particular. Moreover, when you understand that modern wheat was interfered with (pre-GMO, so it escapes that labelling) in the 60’s to 70’s and came into the food chain on about 1980, as explained eloquently by Dr William Davis, the evidence becomes very clear.
And this article entitled The Rats Who Preferred Sugar Over Cocaine includes the following (thanks, Sean):
intense sweetness “is much more rewarding and probably more addictive than intravenous cocaine.” Or, to put it another way, the French scientists’ findings “clearly demonstrate that intense sweetness can surpass cocaine reward, even in drug-sensitized and drug-addicted individuals.”
End of quote.
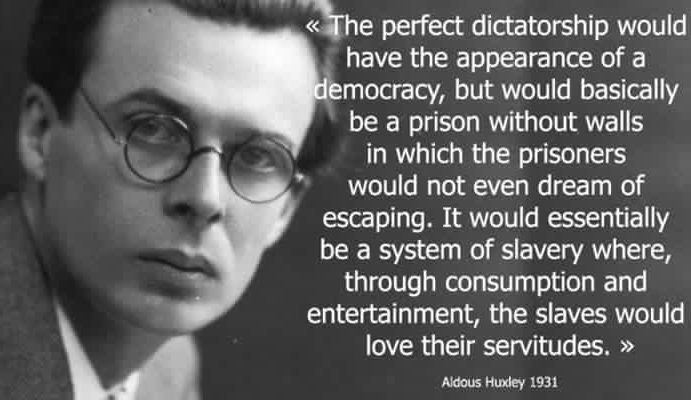
Did you know that? Funny that. Do you think the food industry and those who own and run it didn’t know that? I’ve seen evidence they’ve known it for over 50 years. So, we are intentionally steered towards the foods that make us fat and diabetic whilst told the dead opposite. Our world is full of such examples in almost every area of life. In fact, if it’s strongly advocated by the mainstream, whatever it is, look carefully and suspiciously at it.
And in What if there was a cure for Alzheimer’s disease and no one knew?, Dr. Mary Newport shares the following:
My husband Steve, age 58, has had progressive dementia for at least five years. He had an MRI in May 2008 showing a diffuse involutional change of the frontal and parietal lobes and moderate left-sided and severe right-sided amygdala and hippocampal atrophy with no ischemic change, which would support a clinical diagnosis of Alzheimer’s Disease. For non-medical people, this means that he has shrunken areas of the brain.
Many days, often for several days in a row, he was in a fog; couldn’t find a spoon or remember how to get water out of the refrigerator. Some days were not so bad; he almost seemed like his former self, happy, with his unique sense of humor, creative, full of ideas.
One day I would ask if a certain call came that I was expecting and he would say, “No.” Two days later he would remember the message
from so-and-so from a couple of days earlier and what they said. Strange to have no short-term memory and yet the information was
filed somewhere in his brain. My gut feeling is that diet has something to do with the fluctuation, but what. I knew that he was locked
up in there somewhere, if only there was a key to open up the areas of his brain that he didn’t have access to.
Steve has a BSBA in accounting, and did billing, bookkeeping and accounting for my neonatology practice from home, so that he
could stay with our girls. He loved computers and was a fast typist. He could open computers up to repair them and fix practically anything else without ever having instruction. If he did not have a tool to do something he would “invent” it and make a usable prototype. He loved to kayak and made an attachment to keep his kayak moving in a straight line. About five years ago he began to have trouble organizing to do his accounting work. He would procrastinate as much as possible. He made mistakes with the payroll and I began to sit with him to help him get it right. I thought it was just that our practice had gotten more complicated with more employees. He knew that something was wrong and depression set in. We took him to a neurologist about 4 years ago, who did a Mini Mental Status Exam (MMSE,)
and Steve scored a 23 out of 30, putting him into the mild range of dementia. On this test, the lower the score is, the worse the dementia. His MRI was reported as normal at that time.
About three years ago, Steve started taking Aricept and two years ago Namenda. We were hopeful that, if we could slow his decline enough, a treatment would come along that would turn things around for him. He was changed over from Aricept to Exelon in August 2007 after losing ten pounds over several weeks. In the past 12 months there was a noticeable change. He can no longer cook
for himself, remember to eat a good meal, use a calculator or even perform the simplest addition, however he still keeps busy all day working in the yard or in his garage and he is still in good physical condition. I now do all the cooking for a man who used to cook for his family regularly. I give him the medications because he can’t remember to take them, much less take the right pills. Every night,
we hold each other before we go to sleep and I wonder how many more times we will get to do this. It has been a nightmare to watch his decline and feel helpless to do anything but watch it happen. He is fully aware of his dementia, and we talk about it frequently. He is no longer depressed, probably with the help of counseling, Lexipro and Wellbutrin, or maybe worsening of his disease.
I subscribe to various alerts and check the website www.clinicaltrials.gov periodically to look for drug studies that he may qualify for. Two years ago we tried to get him into a study for a promising anti-inflammatory drug, Flurizan, but he did not qualify because he had a history of depression within the previous two years. Wouldn’t you be depressed if you knew you had Alzheimer’s? In fact, depression may be a symptom or precursor of Alzheimer’s.
Until very recently, I didn’t see anything regarding the potential use of medium chain triglycerides (MCT oil), or ketone bodies (also called ketoacids,) the end product of their metabolism, which may not only treat, but also prevent Alzheimer’s disease. Further, this is a potential treatment for Parkinson’s disease, Huntington’s disease, multiple sclerosis and amyotrophic lateral sclerosis (ALS or Lou Gehrig’s disease), drug resistant epilepsy, brittle type I diabetes, and diabetes type II, where there is insulin resistance. Ketone bodies
may help the brain recover after a loss of oxygen in newborns through adults, may help the heart recover after an acute attack, and may shrink cancerous tumors. Children with drug resistant epilepsy sometimes respond to an extremely low carbohydrate ketogenic diet…
…What do these entities have in common? Our cells can use ketone bodies as an alternative fuel when glucose is not available. (My emphasis). Brain cells, specifically neurons, are very limited, more limited than other cells, in what kinds of fuel they can use to function and to stay alive. Normally, they require glucose (sugar), but they can also use ketone bodies. Humans do not normally have ketone bodies circulating and available to the brain unless they have been starving for a couple of days or longer, or are consuming a ketogenic (very low carbohydrate) diet, such as Atkins. In Alzheimer’s disease, the neurons in certain areas of the brain are unable to take in glucose 4, 5 due to insulin resistance and slowly die off, a process that appears to happen one or more decades before the symptoms become apparent. If these cells had access to ketone bodies, they could potentially stay alive and continue to function…
… At the time of this writing it has been 60 days since he started taking coconut oil (May 21, 2008.) He walks into the kitchen every morning alert and happy, talkative, making jokes. His gait is still a little weird. His tremor is no longer very noticeable. He is able to concentrate on things that he wants to do around the house and in the yard and stay on task, whereas before coconut oil he was easily distractible and rarely accomplished anything unless I super vised him directly, a source of some contention between us!
End of quote.
So, almost by accident, Dr. Newport discovered that after adding natural fats (coconut oil) into her husband’s diet, his Alzheimer’s began to recede. Clearly another disease caused by our high sugar, low fat diets.
But I highlighted the ketone bodies observation above because I think there is a key message here. Conventional wisdom is our brains need sugar (glucose) to function, along with a lot of other parts of the body. But the body has an ENTIRELY SEPARATE mechanism for operating, using ketone bodies, which it gets from fats. But in our high sugar world, this mechanism has been hidden.
Now, I’m not advocating no sugar. I eat lots of fruit. We want natural sugars in our diet. It’s what the body knows how to deal with. And get natural fats back into your diet. We’ve been horrendously lied to. You may not like bacon and eggs like I do, but you and I can both eat it and other saturated fat foods without guilt anymore.
Richard
Check out the extraordinary new, life-changing technology at www.magravsplasmaproducts.com
Recent Comments